Why Do Some Embryos Stop Growing During IVF: Understanding the Challenges and Finding Solutions
Starting the IVF journey is a mixture of hope, anxiety, and a thousand unanswered questions. Although many infertile couples have achieved their dream of having a child with the help of this method, they may have faced challenges along the way. One of the challenges that couples may face in the IVF process is that some embryos do not develop after in vitro fertilization. Research shows that approximately 60% of fertilized eggs in the IVF process develop into blastocysts (high-quality 5-day-old embryos suitable for transfer to the uterus), and the development of the remaining embryos stops before this stage. On the other hand, some blastocyst embryos can also not implant and become healthy pregnancies. Embryo failure can have various causes. Embryo development usually stops due to chromosomal problems or poor egg or sperm quality. During the IVF process, the doctor tries to obtain more eggs to form more embryos by appropriately stimulating the ovaries, so that if some embryos stop developing during the process, there will be other healthy embryos for successful transfer.
If you are new to this journey, don’t worry; many couples have successfully navigated this path and overcome its challenges with awareness. In this article, we will explore the reasons why embryos may not develop and discuss ways to prevent this, so you can approach this journey with greater peace and confidence.
Stages of Embryo Development in the IVF Process
In vitro fertilization (IVF) is one of the most effective methods for treating infertility. In this process, an egg and sperm are fertilized together in a laboratory environment, forming a primary embryo cell. The developing embryo continues its initial stages in the lab and is typically prepared for transfer to the mother’s uterus or for freezing after five days. Monitoring and controlling embryo development within the laboratory environment is crucial. Not only does this continuous oversight help in selecting healthy embryos for transfer, but it also plays a significant role in determining the optimal timing for the transfer and increasing the chances of successful treatment. The stages of embryo development in the laboratory include the following:
1. Fertilization
The process of embryo formation begins with fertilization, which occurs when a sperm fertilizes an egg in a laboratory setting. To enhance the chances of embryo formation, the ICSI (Intracytoplasmic Sperm Injection) method is often used, where a single sperm is injected directly into the egg. The cell formed from the fertilization of the egg and sperm is called a “zygote,” and it represents the first stage of embryonic development.
2. Formation of pronuclei
About 16 to 18 hours after fertilization, two pronuclei, one from the egg and the other from the sperm, are observed in the embryo. If the number of these pronuclei is less or more, the embryo is abnormal, and its development stops.
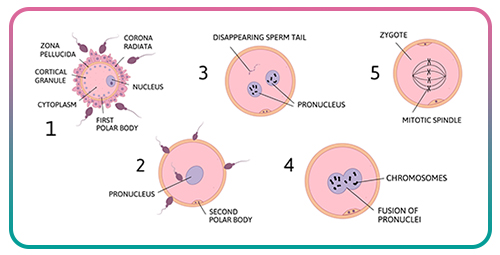
3. Cleavage
Two to three days after fertilization, the primary embryo cell begins to divide, resulting in two, four, or eight smaller cells. These divisions occur without an increase in the overall size of the embryo. If the embryo has not separated by this point, it is considered abnormal and will not develop further. If a biopsy is necessary for genetic testing, such as preimplantation genetic diagnosis (PGD) or sex determination, a cell can be separated from the embryo at this stage for examination. In cases where the doctor does not plan to transfer the embryo to the mother’s uterus after ovulation, the embryos are typically frozen at this stage.
4. Morula Stage
On the fourth day, the embryo reaches the morula stage. During this stage, the morula is a compact mass of cells consisting of a total of 16 cells. This indicates the health and normal development of the embryo.
5. Blastocyst Formation
On the fifth day, the embryo transforms into a blastocyst. The structure of the blastocyst has two important components: the inner cell mass, which will eventually become the embryo, and the outer layer, which will form the placenta. The formation of the blastocyst signifies the ongoing development of the embryo and its readiness for implantation.
6. Blastocyst Transfer
In in vitro fertilization (IVF), embryos are grown in a laboratory until they reach the blastocyst stage. At this point, only the highest quality embryos are selected and prepared for transfer into the uterus. If a blastocyst successfully attaches to the uterine wall and begins to grow, pregnancy occurs.

These stages form the foundation for the creation of new life. For individuals undergoing IVF, understanding these stages can enhance awareness, confidence, and hope. Each stage of embryo development is crucial and must be monitored by an embryologist in a properly equipped laboratory. Progressing through each stage is vital, as it can significantly impact the health of the embryo and its ability to implant and sustain a pregnancy.
What Causes Some Embryos to Stop Growing in IVF?
In vitro fertilization (IVF) is one of the most effective yet complex infertility treatments, often presenting challenges for couples. One significant challenge in IVF is embryo failure. The proper development of embryos is crucial for increasing the chances of successful treatment, implantation in the uterus, and achieving a healthy pregnancy. Therefore, understanding the factors that affect embryo development is vital for screening and preventive measures.
Below, we will explore the reasons that can lead to embryo failure or hinder the formation of embryos during the IVF process.
1. Genetic Factors
Approximately 60% of miscarriages are attributed to chromosomal abnormalities. Therefore, genetic factors significantly influence the development and survival of embryos, both in the laboratory and after implantation in the uterus. These abnormalities typically arise from errors during cell division in the early stages of development and often result in the cessation of fetal growth. Additionally, increasing maternal age and issues with sperm DNA are linked to a higher risk of chromosomal problems, which can reduce the chances of successful embryo development. Some chromosomal abnormalities in embryos that may hinder their growth include:
- Aneuploidy: Aneuploidy is a genetic disorder characterized by an abnormal number of chromosomes in a fetus, either fewer (monosomy) or more (trisomy) than the normal 46 chromosomes. This disorder typically arises from errors during the formation of the egg or sperm in the parents.
- Mosaicism: In mosaicism, an error in cell division results in a fetus with a mixture of cells. Some cells contain the standard 46 chromosomes, while others may have one chromosome less or one extra.
- Structural Abnormalities: Fetal chromosomes can break or become malformed due to various factors, leading to structural abnormalities that can disrupt fetal development.
- Genetic Problems in Parents: Some genetic disorders in the fetus may arise due to inherited genetic issues from the parents.
Preimplantation genetic Diagnosis (PGD) is a crucial tool for diagnosing various genetic issues in embryos, helping to select healthy embryos and enhancing the chances of successful treatment.
2. Poor embryo quality
The quality of the embryo depends on the health and quality of the oocytes and sperm. Factors such as aging, oxidative stress, unhealthy lifestyles, and certain diseases and infections negatively affect the quality of the eggs and sperm.
On the other hand, as the mother ages and ovarian reserve decreases, the number and quality of eggs decrease, reducing the likelihood of forming a healthy, high-quality embryo. Sperm DNA damage and infertility problems in men also reduce the likelihood of blastocyst formation (a stage of embryo development) and can even cause genetic abnormalities in the embryo.
An unhealthy diet, inactivity, smoking, alcohol consumption, chronic stress, and exposure to toxins can also negatively affect the quality of the eggs and sperm and disrupt the proper development of the embryo. Learn more about tips for boosting egg quality: How to improve your egg quality and get pregnant
3. The Adequacy of Endometrial Development for Successful Embryo Implantation
The endometrium, or the inner lining of the uterus, plays a critical role in the success of embryo implantation during in vitro fertilization (IVF). For an embryo to implant effectively and continue developing, the uterine wall must create the right conditions and reach an adequate thickness. If the endometrium fails to achieve the proper thickness during the menstrual cycle, it can obstruct the implantation process and hinder the embryo’s growth. Therefore, it is essential to consult a specialized and experienced doctor for IVF. Ensuring that the uterus is adequately prepared for embryo transfer can significantly enhance the chances of a successful treatment.

4. Uterine Abnormalities
Structural issues in the uterus, such as fibroids, polyps, a bifurcated uterus, endometriosis, and other congenital abnormalities, can hinder implantation. These conditions alter the shape of the uterine cavity or reduce blood flow, creating an unsuitable environment for embryo development. If these abnormalities are accurately diagnosed before embryo transfer, many of them can be treated with procedures like laparoscopy or hysteroscopy.
5. Hormonal Imbalance
Hormonal balance is crucial for preparing the uterus for implantation and ensuring a successful pregnancy. Any imbalance in estrogen and progesterone levels can disrupt the growth of the uterine lining (endometrium) and decrease the chances of successful implantation. Additionally, estrogen and thyroid hormones are essential for the growth and development of the fetus. Disruptions in the secretion of these hormones can hinder fetal growth and may lead to miscarriage.
6. Immune system disorders
In some cases, the mother’s immune system mistakenly identifies the fetus as a foreign agent and prevents its development. Immune disorders can prevent fetal development in various ways, including repeated failure of embryo implantation or even reduced sperm and egg quality, resulting in reduced embryo quality.
7. Laboratory Conditions and Expertise in Embryology
In the IVF process, the environmental conditions of the laboratory greatly influence embryo development. Factors such as temperature, pH level, oxygen concentration, and humidity must be maintained at optimal levels to create the best environment for embryo growth. Additionally, the skill and experience of the embryologist in fertilization, culture, and embryo maintenance play a crucial role in the success of IVF. Therefore, selecting a well-equipped, advanced treatment center with experienced specialists is the most important initial step in the infertility treatment process.
8. The doctor’s skill and experience
The doctor’s experience and skill in preparing the uterus, transferring the embryo, and determining the appropriate time are important for the success of IVF. Using the correct technique in embryo transfer can increase the chances of successful implantation.
9. Lifestyle
Unhealthy habits, such as smoking, excessive alcohol consumption, poor diet, high stress levels, and exposure to pollution, can negatively impact the quality of eggs and sperm, hindering the formation of a healthy embryo during the IVF process. Research indicates that smoking can reduce the chances of IVF success by up to 34%. Additionally, obesity and chronic stress may disrupt the body’s hormonal balance, preventing proper embryo growth and implantation. Therefore, it is advisable to adopt a healthy lifestyle at least three months prior to starting the IVF process to enhance the likelihood of developing a quality embryo. Learn more about foods that help you increase your chances of conceiving: Tips for a healthy pre-pregnancy diet
Effective Strategies for Embryo Growth in IVF
In recent years, significant advancements have been made in the IVF process, which have increased the chances of success and enhanced the patient experience. Below, we will explore the key new strategies and technologies that effectively promote IVF success and support embryo growth.
1. Genetic Testing (PGD/PGS)
Preimplantation genetic Diagnosis (PGS and PGD) is used to screen for chromosomal abnormalities in embryos before they are transferred to the uterus. With these tests, embryologists can identify embryos that have the correct number and structure of chromosomes, thereby reducing the risk of miscarriage. As a result, the chances of successful embryo development, a healthy pregnancy, and the birth of a healthy baby are significantly improved.

2. Advanced Laboratory Techniques
Recent advancements in IVF technology have significantly transformed infertility treatments, playing a crucial role in enhancing fetal development and overall health. These innovations not only improve the chances of a successful pregnancy but also enable doctors and specialists to more accurately monitor critical stages of fertilization and fetal growth. This allows for more informed decision-making throughout the process.
- One of these technologies is time-lapse imaging. This method enables continuous and uninterrupted observation of the stages of embryo development, eliminating the need to remove the embryo from the culture medium. With this technique, embryologists can select the best embryo for transfer based on its growth and cell division, which increases the likelihood of successful implantation and pregnancy.
- EmbryoGlue is an advanced tool designed to mimic the natural compounds found in the uterus, which helps embryos attach more effectively to the uterine wall. Additionally, culture media enriched with essential nutrients and growth factors create optimal conditions for embryo development in the laboratory.
- Another crucial aspect is the quality of the laboratory environment. Factors like stable temperature, good air quality, lack of chemical and microbial contamination, and the use of modern equipment and up-to-date fertilization techniques directly influence the development and survival of embryos. Therefore, selecting a clinic with advanced laboratories that adhere to high-quality control standards can significantly impact the success of IVF.
3. Consultation with an experienced doctor
It’s essential to consult with a specialized and experienced doctor during the IVF process. The skill and experience of the physician in preparing the uterus and selecting the optimal location for embryo implantation play a crucial role in the success of IVF. By using precise ultrasound techniques to examine the thickness and texture of the endometrium and assess the blood supply to the uterus, an experienced doctor can determine the best timing and location for embryo transfer. This careful decision-making can significantly influence the outcome between an unsuccessful cycle and a successful pregnancy. Therefore, choosing a dedicated specialist is a fundamental step in infertility treatment and should be done with thorough consideration and awareness.
4. Improving Your Lifestyle for IVF Success
Adopting a healthy lifestyle is essential for increasing the chances of success with IVF. A diet rich in antioxidants, healthy fats, and protein, particularly the Mediterranean diet, can significantly enhance both egg and sperm quality.
Certain supplements, such as CoQ10, DHEA, and folic acid, have been scientifically proven to improve egg quality. It’s also important to avoid smoking and alcohol, limit caffeine intake, and ensure you are getting enough sleep, as these factors can positively affect embryo implantation success. Learn more about tips for boosting your chances of IVF success: How to increase your chances of IVF success?
Engaging in activities like yoga and meditation, along with psychological counseling, can help reduce stress, regulate hormones, and promote mental readiness, ultimately increasing the likelihood of successful treatment.
5. Using Alternative Methods
For couples who are struggling with serious problems with the quality and quantity of their eggs and sperm, using alternative methods can be very effective. In cases where the couple has a low ovarian reserve due to old age, menopause, certain diseases, and genetic abnormalities, IVF with donor eggs can significantly increase the chances of IVF success. Egg donors are young, healthy women with high egg quality who voluntarily donate their eggs to infertile couples.
If poor sperm quality or azoospermia is the cause of infertility, using donor sperm can help create a high-quality embryo and make IVF successful.
If low sperm quality or azoospermia is contributing to infertility, using donor sperm can help create a high-quality embryo and improve the chances of a successful IVF procedure. In Iran, donation services are legal and widely recognized. These services are carried out with high precision and quality at reputable infertility treatment centers across the country. As a result, the success rate of IVF using donor eggs at the best fertility treatment centers in Iran is approximately 60%.

Why do some embryos fail to grow after being retrieved from the freezer?
First, it is not uncommon for some embryos to fail to grow after being thawed during IVF, and many couples experience this problem. There are several reasons for this:
-
Inherent quality of the embryo
Embryos that are genetically abnormal or of lower quality may not be able to grow after being thawed. This is more common in embryos with chromosomal problems.
-
Stress from Freezing and Thawing
The processes of freezing and thawing can put stress on embryo cells. While advanced freezing techniques are utilized, not all embryos are equally resilient to these processes. Generally, embryos of lower quality are more susceptible to this stress.
-
Laboratory conditions
The conditions in the laboratory play a crucial role in the survival of embryos after thawing. Factors such as the freezing method, the duration and temperature of freezing, and the quality of the materials used can significantly impact outcomes. Therefore, it is essential to choose a laboratory carefully and thoughtfully.
But don’t worry! This doesn’t mean there’s a serious problem or that the couple can’t get pregnant. In fact, the fact that some embryos stop growing after thawing helps specialists select the best and healthiest embryos for transfer, increasing the chances of IVF success.
In short
With advancements in science, the dream of having healthy children is becoming more attainable for couples facing fertility challenges. However, the journey through infertility treatment is often not straightforward and may come with various obstacles and concerns. By educating themselves and seeking guidance from experienced specialists, couples can navigate these challenges more effectively. One significant challenge is the failure of embryos to develop during the IVF process, which often stems from issues such as poor egg and sperm quality or genetic abnormalities in the embryo. To improve embryo quality and enhance the chances of successful growth and implantation, couples can consider lifestyle changes, utilize genetic screening techniques, and, in some cases, explore alternative methods such as egg or sperm donation.
Selecting a treatment center with advanced embryology laboratories and experienced doctors and IVF specialists is essential for developing high-quality embryos. This, in turn, supports the proper and timely transfer of the embryo to the mother’s uterus, which is crucial for healthy development during the IVF process. For more information about the best-equipped fertility treatment centers in Iran, please feel free to contact us.
References:
Study Finds Why Many IVF Embryos Fail to Develop
Day 3 To Day 5 Embryo Freezing & Transfer Survival Rates
Methods to improve frozen-thawed blastocyst transfer outcomes- the IVF laboratory perspective